Medicare integrity contractors medtrainer answers – Medicare Integrity Contractors (MICs) and their indispensable ally, MedTrainer, stand as formidable guardians against Medicare fraud and abuse. MedTrainer empowers MICs to detect and investigate suspicious activities with unparalleled precision, safeguarding the integrity of this crucial healthcare program.
MICs are tasked with the critical mission of identifying and preventing Medicare fraud and abuse, ensuring the judicious use of taxpayer funds. MedTrainer serves as their steadfast companion, providing an advanced platform that analyzes vast amounts of data to pinpoint potential anomalies and red flags.
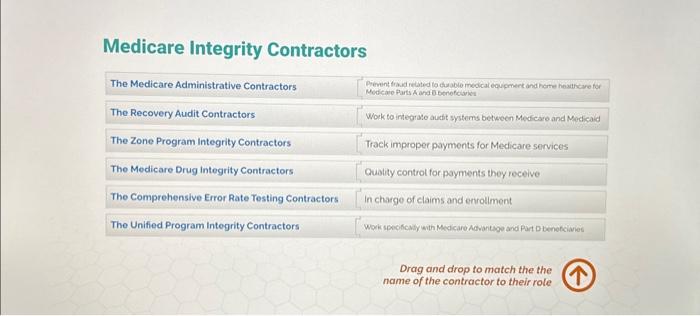
Medicare Integrity Contractors (MICs)
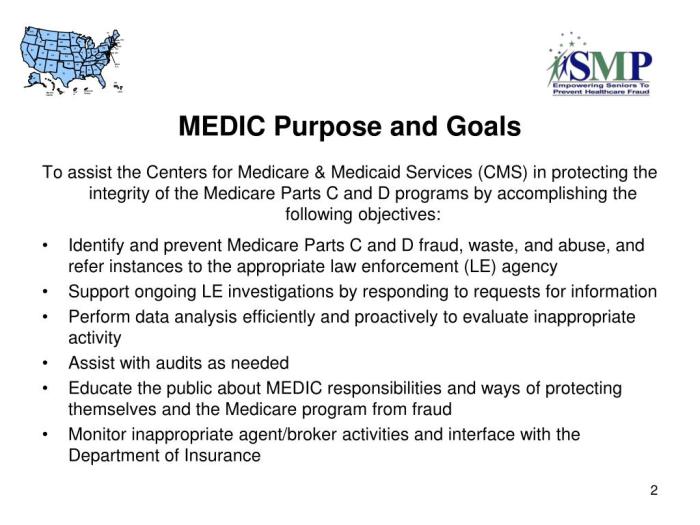
Medicare Integrity Contractors (MICs) are private organizations that are contracted by the Centers for Medicare & Medicaid Services (CMS) to help detect and prevent Medicare fraud and abuse.
MICs play a vital role in protecting the integrity of the Medicare program by reviewing claims, conducting investigations, and taking action against providers who are suspected of committing fraud or abuse.
Role of MICs in Detecting and Preventing Medicare Fraud and Abuse, Medicare integrity contractors medtrainer answers
MICs use a variety of methods to detect and prevent Medicare fraud and abuse, including:
- Reviewing claims data to identify potential fraud and abuse patterns
- Conducting investigations of providers suspected of committing fraud or abuse
- Taking action against providers who are found to have committed fraud or abuse, including recommending that CMS exclude them from the Medicare program
Common Fraud and Abuse Schemes Targeted by MICs
MICs target a variety of fraud and abuse schemes, including:
- Billing for services that were not provided
- Billing for services at a higher rate than is allowed
- Submitting false or misleading claims
- Offering or receiving kickbacks or bribes
- Falsifying medical records
MedTrainer
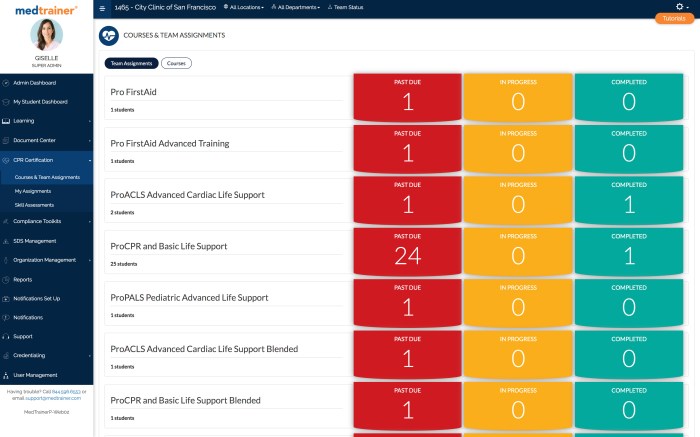
MedTrainer is a software tool that is used by MICs to help them identify and investigate potential fraud and abuse cases.
MedTrainer uses a variety of data sources, including claims data, provider data, and beneficiary data, to identify potential fraud and abuse cases.
MedTrainer can also be used to track the progress of investigations and to generate reports on fraud and abuse trends.
Key Features and Capabilities of MedTrainer
MedTrainer has a number of key features and capabilities, including:
- The ability to identify potential fraud and abuse cases based on a variety of data sources
- The ability to track the progress of investigations
- The ability to generate reports on fraud and abuse trends
- The ability to share data with other MICs and with CMS
Answers for MedTrainer
Frequently Asked Questions (FAQs)
What is MedTrainer?
MedTrainer is a software tool that is used by MICs to help them identify and investigate potential fraud and abuse cases.
How does MedTrainer work?
MedTrainer uses a variety of data sources, including claims data, provider data, and beneficiary data, to identify potential fraud and abuse cases.
What are the benefits of using MedTrainer?
MedTrainer can help MICs to identify and investigate potential fraud and abuse cases more quickly and efficiently.
How can I get access to MedTrainer?
MICs can access MedTrainer through the CMS website.
MICs and MedTrainer Collaboration: Medicare Integrity Contractors Medtrainer Answers
MICs and MedTrainer work together to help detect and prevent Medicare fraud and abuse.
MedTrainer provides MICs with the tools and data they need to identify potential fraud and abuse cases.
MICs use MedTrainer to track the progress of investigations and to generate reports on fraud and abuse trends.
The collaboration between MICs and MedTrainer has helped to improve the efficiency and effectiveness of Medicare fraud and abuse detection.
Benefits of Using MedTrainer for Medicare Fraud and Abuse Detection
There are a number of benefits to using MedTrainer for Medicare fraud and abuse detection, including:
- Increased efficiency and effectiveness of fraud and abuse detection
- Improved ability to track the progress of investigations
- Enhanced ability to generate reports on fraud and abuse trends
- Improved collaboration between MICs and CMS
Case Studies and Examples
Case Study: MedTrainer Helps MIC Identify $1 Million in Fraudulent Claims
In one case, MedTrainer helped a MIC identify over $1 million in fraudulent claims submitted by a provider.
The MIC used MedTrainer to analyze claims data and identify a pattern of suspicious billing.
The MIC then investigated the provider and found that they had been submitting claims for services that were not provided.
The MIC took action against the provider and recommended that CMS exclude them from the Medicare program.
Question Bank
What is the primary purpose of Medicare Integrity Contractors (MICs)?
MICs are responsible for detecting and preventing fraud, waste, and abuse within the Medicare program, ensuring the appropriate use of taxpayer funds.
How does MedTrainer assist MICs in their investigations?
MedTrainer provides MICs with advanced data analytics capabilities, enabling them to identify potential fraud and abuse cases with greater accuracy and efficiency.
What are some common fraud and abuse schemes targeted by MICs?
MICs focus on various fraud and abuse schemes, including billing for services not rendered, upcoding procedures, and submitting false claims.
How has MedTrainer impacted the effectiveness of MIC investigations?
MedTrainer has significantly enhanced the efficiency and accuracy of MIC investigations, leading to substantial savings for the Medicare program.